
Recently I received a lengthy email from a longtime friend who is undergoing treatment for cancer. He was open and honest about wondering whether to continue the therapy, he was very tired and wondered if it was worth it to keep fighting. He had now made the decision to continue with it, because his wife whose health has not been good in recent years needs him. I sent him the following response:
Thanks so much (for sharing the details of what he has been going through). I will pray more specifically, and particularly target the pain and horrible discomfort you are going through. THROUGH, the key word, through to the other side.
The following is long, sorry, but read it gradually if you need to. Put it off till later if you need to.
One thing you said – “You would not believe what this chemo does to a person’s temperament” – yes, I do believe it.
2011 was a very different year for me. I’d had a normal mammogram in December 2010, but then they called me to come in for more films. The eagle-eye technician had spotted an enlarged lymph node deep under my left arm. After those films they recommended a needle biopsy, from which I bled, and bled, and bled. I went home wrapped up like a mummy to stop the bleeding. Thankfully my daughter Shelby was driving me!
The lab report showed breast cancer type cells in the lymph node. Because there was no tumor in the breast itself, it took weeks’ worth of other testing to find the small tumor attached to that lymph node. I met and talked to lots of technicians while undergoing MRI, full body bone scan, PET scan, and lots of blood work. I got to pray with and for many of them.
Well, since this little tumor involved the lymph system, the cancer was already Stage 3, the oncologist Dr. Bajaj explained. He was so patient and kind, explaining everything, answering my every question.
And so beginning the end of January 2011 I underwent 5 months of chemotherapy for breast cancer, with every bad side effect you can get. All the skin peeled off my face, hands and feet. Shingles developed across my chest, side and back, twice. Pain – in my case, not from the cancer but from the treatment. I needed several “vacations from therapy” during those months to allow the side effects to subside, before beginning again.
Soon weakness, fatigue, and exhaustion hit me, even when I had done absolutely the minimum of moving around. I set up a line of dining room chairs from my bed to the bathroom and kitchen, because I could only take a couple of steps before needing to sit down and rest. I was living alone and only had one cat then, Friday, my faithful gentlemanly furry companion who stayed quietly by my side all that time. (See photo.) I ate little, mainly TV dinners or canned soup. No appetite.
The chemo was followed by mastectomy surgery, where accidentally they tore a bursa in my left shoulder. More pain, and the shoulder problem could not be repaired so it’s still there.
After the surgery, I developed a seroma – where the breast tissue had been removed, lymph fluid gathered in a large pool, creating the effect of a tumor pressing on my heart and lungs. I had to go back to the hospital to have that drained the first time, to the doctor’s office the second and final time. The seroma wasn’t painful in itself, it just caused a lot of trouble breathing. They let me watch the LONG needle sticking into my chest on the fluoroscope, at my request. I could not bear to look at the needle, but the screen was interesting to watch. Immediately I felt better and could breathe deeply again.
All that was followed by over 20 rounds of radiation, where I developed severe excruciating radiation burns across my chest and neck, and it basically destroyed my thyroid. I finally told the radiation doctor to just stop the radiation, and he reluctantly agreed although I still had 6 or 7 more to go. I asked would those make any substantial difference in my survival chances? And he just shrugged and said, probably not. He was nice, but I was glad to say goodbye to that department.
During all those month I had almost no contact with any non-medical people. The one church “friend” who drove me to the hospital one day told me that God had done this, to provide a testimony to other people. I disagreed, not angry at him but at the enemy, the chief of liars, who had deceived him into not fighting that battle of faith at all. His wife was also being treated for breast cancer at the same time and he told everybody that God had given her cancer so she could witness to people in the hospital. I decidedly disagreed and told him so. I politely declined any of his further offers to drive me.
One Cancer Society volunteer driver was outspoken and rude about why I called them for help, when I had a perfectly good car in my driveway. I never called them again, either. I just gritted my teeth, moved slowly, and drove myself to the hospital for therapy every time after that. It wasn’t fun, but I worked out a way to make it doable for me. A couple of steps, stop and rest. Another couple of steps, stop and rest. I always prayed for a parking space close to the door, and they always were. 😊 There was no valet parking at the Cancer Center, unfortunately.
My temperament during that time became very different, for me. I became stubborn, determined, and changed my way of speaking. I told every cancer cell in my body to “Shrink, shrivel, die and disappear,” and said so to all my doctors. I insisted that each one write that in my chart. I also asked each one to allow me to pray for them, to lay hands on them (or hold hands with them if they preferred) and pray. Every single one agreed, even Dr. Bajaj who has no religion, according to him. He was raised in a Hindu home but didn’t adopt that religion. When I asked him, he said, “But I’m not a Christian.” I said, that’s okay, I am. And so he allowed me to hold his hand and pray for him. At one checkup he asked with a smile, “Are you still speaking to your body?” I smiled back and said, “Oh yes, always!”
My prayers with and for each physician, nurse and therapist were simply that the Lord would bless them, would use them in their work to help me and all their other patients to heal, and that Father God would be close to them personally so that they would know, KNOW, who he was and how much he loved them. I still pray for and with my doctors to this day. One cardiologist asked me to pray for his nurse who was out at the desk, as she was having a bad day. He said please not to let her know he’d asked me. As I left, I just stopped by her desk, noticing how glum she seemed. I asked if I could pray for her. She agreed, and I did. She was smiling a little when I left.
On days when I was able to get out of bed and sit at my computer, I searched for and began watching videos of revival and miracle healing services around the world. Dozens, maybe even hundreds of them, from Wales in the UK to Australia, even Europe where the messages had to be translated into the local language and so those services were very, very long! I watched some of the live broadcasts late at night or very early in the morning, because of the time zone differences.
I saw people being healed instantly of a great many different diseases and physical ailments, and with every service I watched, my faith grew and strengthened. My stubbornness and determination grew too. I was also angry, but at the right personality – the lying, destroying enemy of our faith and our lives. I learned how to take authority better over him, and over my responses to his attacks. I learned how to talk life, not death! John 10:10 became my life verse that year and it still is.
So I do get it, about the temperament. I understand the stress, the mental and emotional stress in addition to all the physical stress. The people you meet are not ALL pleasant, not even the nurses and therapists. But Father God is. For that I was and am very grateful! He led me a life and work of intercessory prayer during that year, as I saw so many other patients and their families struggling, and many medical personnel also struggling to do their hard jobs. Some were wonderful to me, some were abrupt and impatient. They all needed prayer!
Most of my family and friends could not truly understand, even though they wanted to help in some way. For a long time I was not allowed to be around people outside the hospital because of my depressed immune system, so people would bring food to the door, ring the doorbell and leave a box outside the door. I would rather they had just prayed and not done that, it required me to get out of bed, get slowly down the hallway, open the door, pick up whatever it was and bring it in. Shelby was the exception, she could just bring whatever I needed, come inside and do whatever I needed, without my having to get out of bed.
2011 was a very different year. I learned a lot, about myself, about how great our God is, His word, and what His will is for me, and for you – Life, and that more abundant.
Love always,
Bette
 (Reblogged from Esther’s Petition July 24, 2019)
(Reblogged from Esther’s Petition July 24, 2019) My most recent blood work was all really good, except for a slightly higher than normal cholesterol level. It is now 20 points lower than last year, however, so I’m happy with it. (I don’t take medication for that; it gave me horrible nightmares.)
My most recent blood work was all really good, except for a slightly higher than normal cholesterol level. It is now 20 points lower than last year, however, so I’m happy with it. (I don’t take medication for that; it gave me horrible nightmares.) A few days after the echo was done I also had a follow-up stress test, recommended but not gotten at my last checkup with Dr. Wall. (At the time it was first scheduled I came down with a cold, followed by bronchitis. Coughing didn’t seem conducive to getting a good test, so I had skipped having it done then.)
A few days after the echo was done I also had a follow-up stress test, recommended but not gotten at my last checkup with Dr. Wall. (At the time it was first scheduled I came down with a cold, followed by bronchitis. Coughing didn’t seem conducive to getting a good test, so I had skipped having it done then.) My 6 months FU with cardiologist Dr. Wall was this morning and he was very pleased with my overall improvement. He congratulated me on my progress, saying he didn’t think he himself could keep to the whole foods, plant-based program I’m on – he loves chicken too much! Can’t give up the chicken. He added that he didn’t eat it fried any more, so that was something.
My 6 months FU with cardiologist Dr. Wall was this morning and he was very pleased with my overall improvement. He congratulated me on my progress, saying he didn’t think he himself could keep to the whole foods, plant-based program I’m on – he loves chicken too much! Can’t give up the chicken. He added that he didn’t eat it fried any more, so that was something. My blood pressure has steadily improved, so much so that several weeks ago I was able to completely discontinue Lorsartan, switching Metoprolol to mornings at a dose of 25 mg. I probably won’t even need that much longer. My weight is down to 168, my clothes are all feeling pretty baggy and even my shoes are loose.
My blood pressure has steadily improved, so much so that several weeks ago I was able to completely discontinue Lorsartan, switching Metoprolol to mornings at a dose of 25 mg. I probably won’t even need that much longer. My weight is down to 168, my clothes are all feeling pretty baggy and even my shoes are loose. “Dr. Caldwell Esselstyn of Cleveland Clinic called me again and we talked for about 30 minutes. (See
“Dr. Caldwell Esselstyn of Cleveland Clinic called me again and we talked for about 30 minutes. (See  Since taking authority over my eating lifestyle, observing and following the advice of physicians at the Cleveland Clinic and elsewhere, I have discovered increased energy and stamina, lower blood pressure, no shortness of breath, improved lab work in every area, and I have lost 17 pounds so far.
Since taking authority over my eating lifestyle, observing and following the advice of physicians at the Cleveland Clinic and elsewhere, I have discovered increased energy and stamina, lower blood pressure, no shortness of breath, improved lab work in every area, and I have lost 17 pounds so far. 
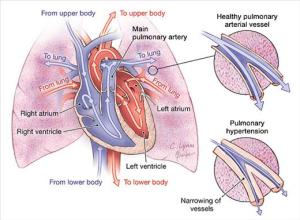 It was just an ordinary echocardiogram. There are many different measurements, and diagnosis is based on certain readings – size of heart chambers, pressure within the chambers, etc.
It was just an ordinary echocardiogram. There are many different measurements, and diagnosis is based on certain readings – size of heart chambers, pressure within the chambers, etc.